Abstract
INTRODUCTIONThe use of surrogate endpoints such as progression-free survival (PFS) and other time-to-event (TTE) endpoints is common in multiple myeloma (MM) clinical trials. However, the validity of these alternative endpoints as surrogates for overall survival is not consistently proven in most malignancies, including MM, and requires further investigation. Furthermore, relapses in MM may occur clinically (with the appearance of new lytic lesions or extramedullary disease) or biochemically, with a rise of a monoclonal protein. As clinical progression may be more prognostically relevant than asymptomatic biochemical progression, it is important for clinical trials to include the nature of progression as part of their results. For all randomized trials that used a primary or co-primary time-to-event endpoint such as PFS, event-free survival (EFS) and time-to-progression (TTP), we assessed whether progression was reported as a biochemical progression or a clinical progression and whether a benefit in PFS translated to an OS benefit upon extended follow-up. We also performed a surrogacy analysis of PFS for OS in these trials to evaluate the strength of surrogacy.
METHODS Three databases were searched (MEDLINE/PubMed, Embase, and Cochrane Registry of Controlled Trials) for all RCTs in MM from 2005 to 2019. The primary objectives of this study were twofold, to evaluate the proportion of RCTs using time-to-event endpoints that reported whether progression was biochemical and/or clinical, and to evaluate the strength of surrogacy of PFS to OS for all RCT's that used PFS as a primary or co-primary endpoint. We used an unadjusted linear regression to evaluate the association between OS HR and PFS HR for studies reporting time-concurrent numbers, or for studies reporting OS at a later follow up, and to calculate the coefficient of determination (R2). We also calculated Pearson's correlation coefficients and 95% confidence intervals for the correlation coefficients. We classified the strength of association as weak (r ≤ 0.7), medium (r > 0.7 to r < 0.85), and strong (r ≥ 0.85).
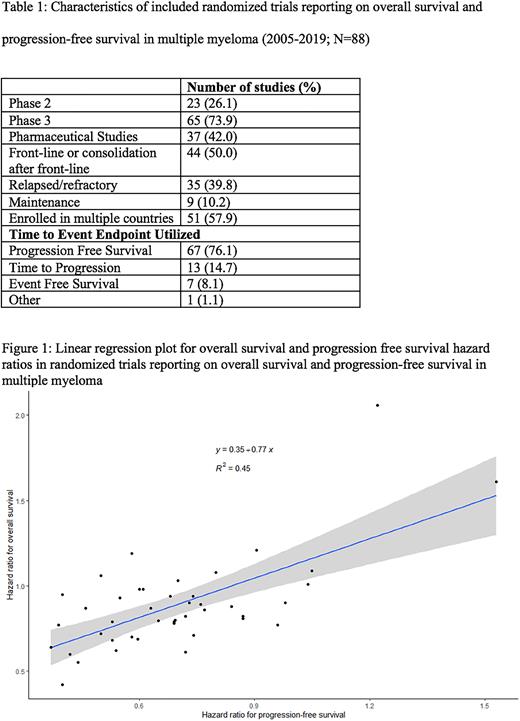
RESULTS The initial search strategy yielded 1171 results. After searching conference proceedings and excluding duplicates or studies not meeting inclusion criteria, 151 discrete RCTs were included. When substratified for only those trials that were primarily evaluating time-to-event endpoints, a total of 88 studies were identified, of which 67 had PFS as either a primary or co-primary endpoint. A total of 45 studies included HR for both PFS and OS, allowing for regression analysis. Table 1 lists characteristics of included studies.
We found only one study that described whether progression events were biochemical or clinical. Two additional studies reported time to first skeletal event and renal impairment reversal respectively but did not clearly differentiate between biochemical and clinical progression.
Amongst the 45 studies where correlation could be assessed, the R2 from the regression model suggested that among the variance in OS, 45% was explained by PFS (Figure 1). The correlation between PFS and OS was 0.67 (95% CI 0.47-0.81), indicating a weak association of PFS with OS.
For newly diagnosed (n=21) studies, 39% of the variance in OS was due to changes in PFS. The correlation between PFS and OS was 0.63 (95% CI 0.27-0.83) indicating a weak association of PFS with OS.
For studies of relapsed/refractory MM (n=20), 60% of the variance in OS was due to changes in PFS. The correlation between PFS and OS was 0.77 (95% CI 0.49-0.91), indicating a medium association of PFS with OS.
CONCLUSION We demonstrate that PFS is characterized poorly in MM trials, with almost no trials identifying whether progression events are biochemical or clinical. Our results show that PFS is a poor surrogate for OS in MM, especially for newly diagnosed disease. This review highlights the need for more comprehensive reporting of progression characteristics in order to establish the magnitude of clinical benefit to our patients. While acknowledging the tremendous improvements in outcomes in patients with MM with the current framework of trials, we highlight that differences in PFS do not reliably predict differences in OS, and we urge caution in attempts to establish surrogacy of other outcomes such as measurable residual disease with PFS.
Disclosures
Sborov:Sanofi: Consultancy; Amgen: Consultancy; Bioline: Consultancy; BMS: Consultancy; Pfizer: Consultancy; Abbvie: Consultancy; GSK: Consultancy, Membership on an entity's Board of Directors or advisory committees; Janssen: Consultancy, Membership on an entity's Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal